Damage to synapses caused by Alzheimer’s disease reversed

Alzheimer’s disease is a progressive, neurodegenerative disorder that is the leading cause of dementia, which involves cognitive decline, memory loss, and ultimately the inability to perform daily tasks. It affects an estimated 55 million people globally, and in Japan alone, an estimated 4.4 million people are living with dementia, a number that is expected to climb to 6.5 million in 2060 according to government data.
Curing or delaying the debilitating symptoms of Alzheimer’s is extraordinarily difficult due to the elusive nature of the disease. The exact cause is unknown, and likely involves multiple factors from genetics to lifestyle, and due to the progressive nature of the condition, it is often too late to treat effectively once the symptoms begin to impact daily life.
However, a team of researchers from the former Cellular and Molecular Synaptic Function Unit at the Okinawa Institute of Science and Technology (OIST), led by Professor Emeritus Tomoyuki Takahashi, has now made headway into finding a viable treatment of those symptoms, putting us on the path to rescuing brain functions before they are irreversibly damaged by Alzheimer’s disease. Their findings have recently been published in Brain Research. “We successfully reversed the symptoms of Alzheimer’s disease in mice,” explains Dr. Chia-Jung Chang, first author of the study and presently a member of the Neural Computation Unit at OIST. “We achieved this with a small, synthetic peptide, PHDP5, that can easily cross the blood-brain barrier to directly target the memory center in the brain.”
Saving dynamin
A central factor in Alzheimer’s disease is the health of brain synapses. Synapses are the junctions between neurons in the brain, where information is conveyed from one neuron to the next through chemical neurotransmitters encased in synaptic vesicles. These vesicles have to be constantly recycled to secure a steady supply, and an essential step in the vesicle recycling process is the membrane retrieval (endocytosis) by the protein dynamin, which ‘cuts off’ the vesicle from the cell membrane. Dynamin is available throughout the neurons, either freely or bound to the microtubules that make up the cytoskeleton of cells.
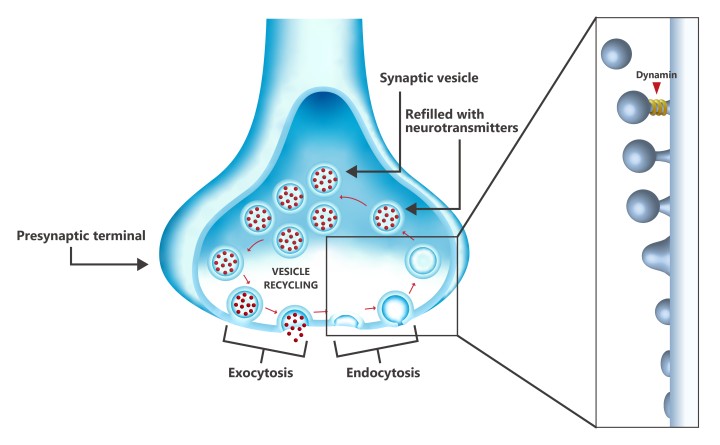
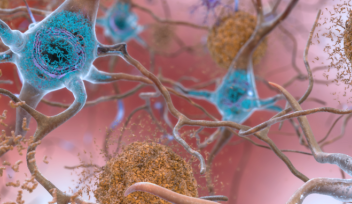
The key antagonist here is the protein tau, which in normal circumstances is involved in stabilizing the microtubules. However, in the early stage of Alzheimer’s, tau begins to disassociate from microtubules. Being freely available, tau over-assembles new microtubules, effectively vacuuming dynamin from cell, making it unavailable for the last step of endocytosis. As Alzheimer’s progresses, the accumulated tau aggregates into neurofibrillary tangles, which are the hallmark of the disease – by the time these tangles show up on brain scans, it is often too late to treat the disease.
The OIST researchers focused specifically on the dynamin-microtubule interaction, and they have previously proven the positive effects of inhibiting this interaction in vitro using the synthetic peptide PHDP5. Dr. Zacharie Taoufiq, presently in the Synapse Biology Unit at OIST and second author of the paper, explains: "By preventing the interaction between dynamin and microtubules, PHDP5 ensures that dynamin is available for vesicle endocytosis during recycling, which can restore the lost communication between neurons inside the synapses at an early stage.”
Using transgenic mice, the researchers have now shown the same restorative effect in vivo. "We were thrilled to see that PHDP5 significantly rescued learning and memory deficits in the mice,” says Dr. Chang. “This success highlights the potential of targeting the dynamin-microtubule interaction as a therapeutic strategy for Alzheimer's disease."

Because PHDP5 inhibits dynamin-microtubule interactions generally, the researchers modified the peptide to include a cell-penetrating peptide, which allows the treatment to be administered through the nasal cavity where the blood-brain barrier is not fully developed, and which is close to the memory center of the brain, the hippocampus. In this way, the peptide would be delivered to the hippocampus at a higher concentration than through other methods of administration, while also minimizing potential side effects elsewhere in the body.
From molecules and mazes to viable treatments
Provided the synapses are treated with PHDP5 at a relatively early stage, the damage caused by the rampant dynamin-microtubule interaction can be reversed to the point that the treated transgenic mice have learning and memory abilities on par with healthy mice. While the peptide cannot cure Alzheimer’s, the inhibition of the dynamin-microtubule interaction delays cognitive decline significantly, to the point where it may not affect healthy people within a normal lifespan.
Emboldened by these results, the research team, now headed by Dr. Taoufiq and composed of specialists from different units across OIST, is continuing their work on the treatment. Dr. Taoufiq, based in the Synapse Biology Unit, is working to improve the peptide itself and the ways in which it functions in vivo. “We want to increase the amount of PHDP5 in the brain to achieve better effects, while minimizing side effects,” as he puts it. Meanwhile, Dr. Chang, based in the Neural Computation Unit, is working to introduce AI in the pursuit of additional and more robust data: “We’re using the different areas of expertise within OIST to improve our research.”
At the same time, the team is working with the OIST Innovation division to move the peptide through the production pipeline. “We want to involve pharmaceutical companies going forward,” explains Dr. Taoufiq. “They have the necessary expertise in pharmacology and the capacity for human trials to turn our peptide into a viable treatment.”
While the journey from research to drug is infamously long, taking an average of 20 years from paper to prescription, the researchers remain highly enthusiastic. As Dr. Chang says, “the coronavirus vaccine showed us that treatments can be rapidly developed, without sacrificing scientific rigor or safety. We don’t expect this to go as quickly, but we know that governments – especially in Japan – want to address Alzheimer’s disease, which is affecting so many people. And now, we have learned that it is possible to effectively reverse cognitive decline if treated at an early stage.”
Comment from OIST Professor Emeritus Tomoyuki Takahashi
While he is now retired from OIST, Prof. Takahashi started the project and ran it until the unit’s closure. “In this study, together with the previous one, we have clarified the pathological significance of dynamin-microtubule (MT) interaction in Alzheimer’s disease (AD), by which synaptic functions are significantly impaired. The dynamin-MT inhibitor PHDP5 rescues synaptic dysfunctions caused by tau accumulation in brain slices and can reverse learning and memory deficits to normal levels in transgenic AD mice models. This in vivo effect is robust since it is reproducible in double-blind tests and consistent in two types of model mice. Clearly, the next crucial step is to submit PHDP5 to the Phase 1-4 tests of AD therapeutic trials, which would be best performed by pharmaceutical companies. We strongly hope that our peptide could go through the tests and reach AD patients without much delay and rescue their cognitive symptoms, which is the primary concern of patients and their families.”
Note
The study began in the Cellular and Molecular Synaptic Function Unit, which was closed in March 2024. Professor Tomoyuki Takahashi designed and directed the whole project and wrote the text of the paper, while group leader Dr. Tetsuya Hori, currently in the Synapse Biology Unit together with Dr. Zacharie Taoufiq, arranged the experimental setups, the animals, and organized collaborations. Dr. Chia-Jung Chang conducted behavioral experiments and Dr. Taoufiq designed and modified the peptides.
Article Information
Specialties
Research Units
For press enquiries:
Press Inquiry Form