The OIST antibody test required an interdisciplinary approach
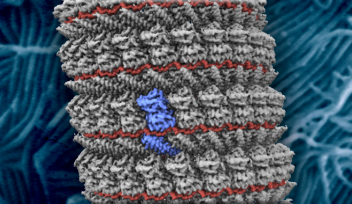
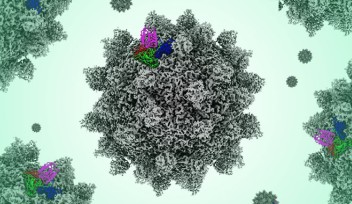
When a person is infected with a virus, their immune system makes antibodies, which help the body to fight the virus. The piece of the virus that the antibody attaches to is called an antigen. For SARS-CoV-2, the spike protein S, which is on the surface of the virus, is one of the main antigens. Antibodies can remain in the blood even after the virus has been killed off, and they can be detected using a method called Enzyme-Linked Immuno Sorbent Assay or ELISA. Thus, it is possible to test healthy individuals to determine if they have been infected and recovered from SARS-CoV-2.

Two-step process ensures accuracy
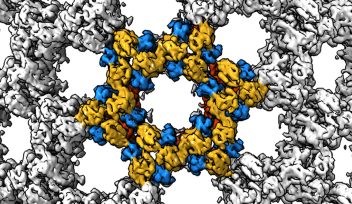
In early March, when the first ELISA assay for SARS-CoV-2 was developed by the Krammer Lab in New York, Professor Matthias Wolf had the plasmids shipped to Okinawa. These plasmids contained the genes that encoded the spike protein and its receptor-binding domain. Professor Wolf had previously done work on the Ebola virus and wanted to try something similar for detecting SARS-CoV-2. His Molecular Cryo-Electron Microscopy Unit set about creating the OIST antibody test.
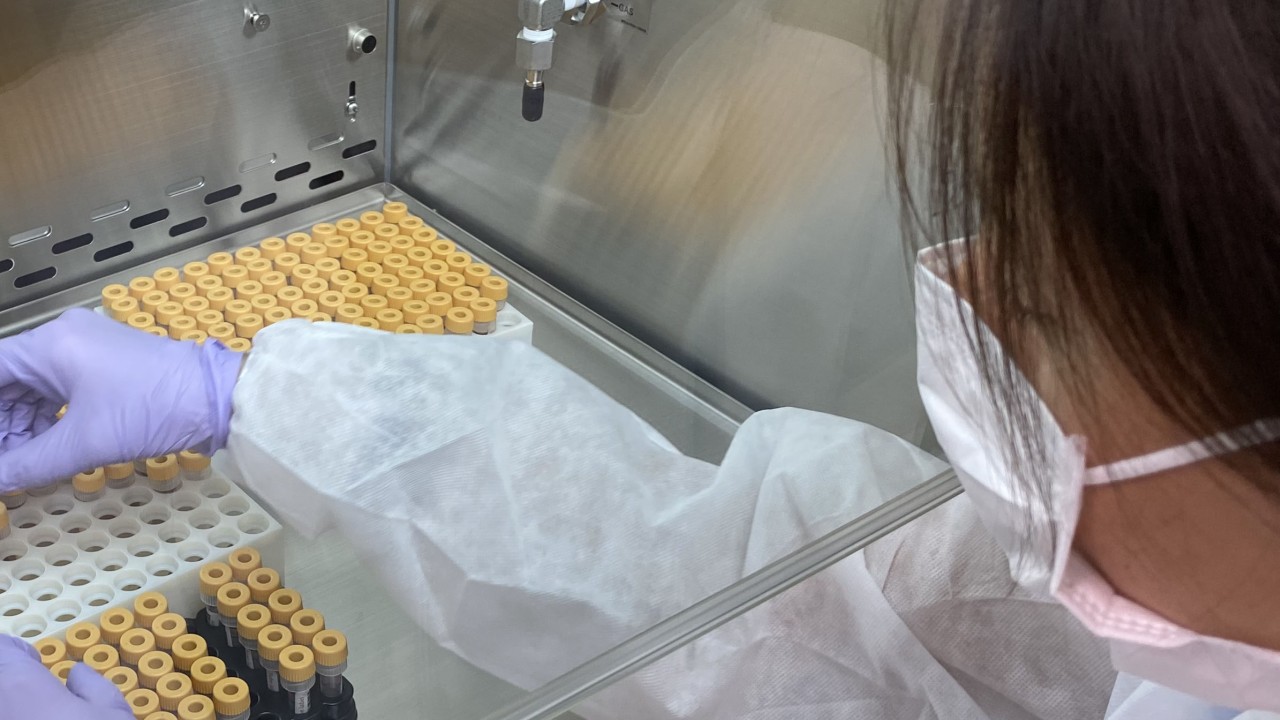
When the ELISA reagents arrived, staff scientist Dr. Tae Gyun Kim started to express and purify the spike proteins. This was necessary to test the samples to see if antibodies were present.
Meanwhile, the researchers also thought about how they would safely inactivate any samples received. “We had to centrifuge to separate the serum and heat the samples,” said staff scientist Dr. Satoshi Shibata. “We used a laboratory with biosafety level 2 containment and a dedicated centrifuge. We inactivated all the samples before we thought about testing them.”
Not all antibody tests are created equal. To maximize the accuracy of the test, the assay used at OIST consists of a two-step process.
The first step used one part of the spike protein to see if there were any antibodies in the sample that would bind to it. This was highly sensitive but not very specific to this virus, meaning that it could detect low levels of antibodies, but they weren’t necessarily from SARS-CoV-2.
“If a serum sample was positive in step one, it was tested again in step two,” said Dr. Melissa Matthews, post-doctoral scholar in the Unit, who, alongside research assistant Noriko Shibata, was in charge of setting up the test. “Step two used the whole spike protein complex and a dilution series of the serum sample. This was highly specific so only samples which had been infected with the virus in the past several months would be positive in this test.”
The researchers showed this accuracy on control samples that they received from outside of OIST. The positive controls were samples that had tested positive for SARS-CoV-2 in PCR tests in April. The negative controls were serum samples from last year that were known not to have SARS-CoV-2 antibodies. In both instances, these controls were included on every assay plate and the test results rang true.
Finally, Christian Butcher, a technician from the Fluid Mechanics Unit, was instrumental in automating the testing process so the capacity could be expanded. Without this automation, the testing would have had to be performed manually, which would have been much less efficient.
Testing the OIST community
One issue with testing the OIST community was that samples needed to be provided without doctors to draw the blood. So, the researchers decided to use finger pricking. They ordered several different kits for this and tested them on themselves. They wanted something that was easy-to-use, safe, and inexpensive. “We ended up making our own kit by ordering individual components,” said Dr. Shibata.
Once the team had settled on the composition of the kit, they thought about the practicalities of testing volunteers anonymously. A QR code system was created and, with the help of the IT section, it was linked to a website, which included an instructional sheet and video. Each sample had a corresponding barcode and QR code. The barcode was left with the sample, whereas the participant kept and scanned the QR code to get their result. No personal information was retained nor required.
The final hurdle involved getting ethics approval. With the help of OIST’s Human Subjects Research Ethics Committee this was granted, and the tests were ready to be used by the OIST community in August 2020 at the onset of the second wave of infections on Okinawa.
“Our team really came together,” said Professor Wolf. “We had to work on a lot of different things – protein expression, ELISA testing, creating a website, QR code, sample and plate barcodes, 3D-printing tube racks, automation. We had people helping from other units across the University. It was really energizing for me and for my unit as a whole.”
Sometimes it proved difficult to extract enough serum from the blood droplet. These results were uploaded to the website as ‘not determined’ and individuals could repeat the test. In total, the researchers looked at 635 samples that were voluntarily given by the OIST community. None of these tested positive for COVID-19 antibodies. Their results have been summarized in a manuscript submitted to the medRxiv pre-print server. In collaboration with medical professionals, they have also tested 300 samples from clinics and a small cluster of infections in Naha. They will now test 6,000 samples from the Okinawan community provided in the scope of a contract with the Okinawan Prefectural Government.




Specialties
Research Unit
For press enquiries:
Press Inquiry Form